The Real Way Pandemics Start And What’s Being Done To Stop The Next One
Pathogen spillovers from animals to humans may be the cause of widespread illness but scientists are still unsure.
This article is more than 2 years old
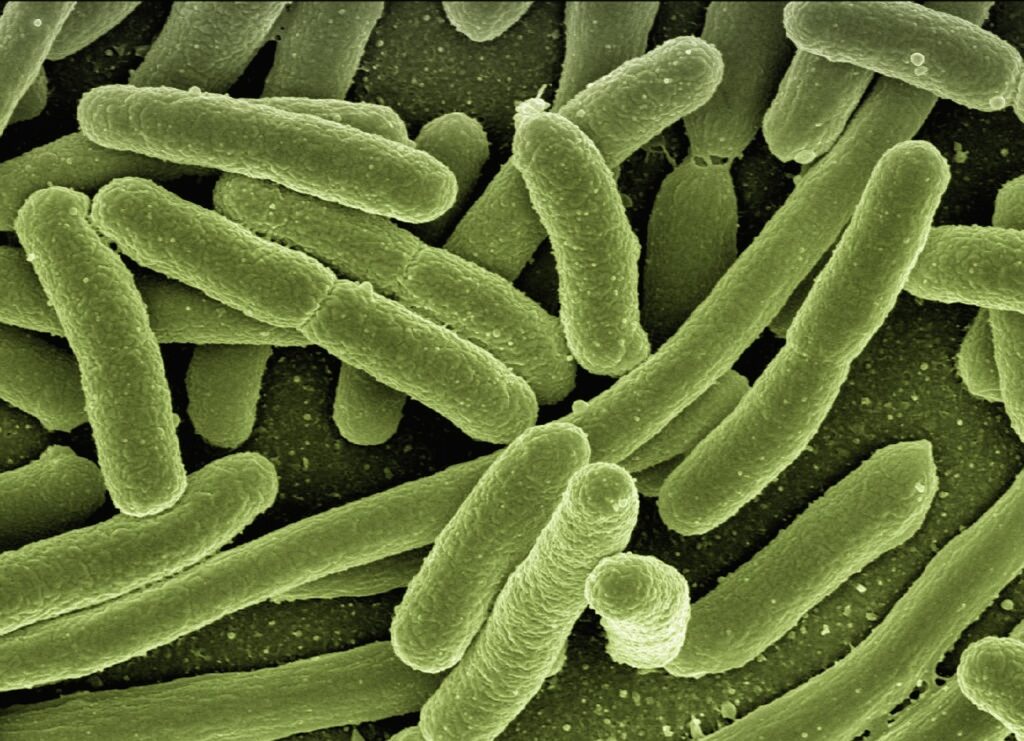
It’s a question scientists have been trying to answer for ages: how do pandemics begin? For decades it’s been believed that rare spillover pathogens—viruses that jump from animals to humans—are behind most widespread disease outbreaks. In recent years, however, virologists and epidemiologists have begun to question this once-accepted theory.
The main problem with the original spillover theory is that the vast majority of animal viruses are only able to infect animals. Only a minuscule number ever make the jump–or spillover–to infect humans, much less cause pandemics. Evolutionary biologist Stephen Goldstein at the University of Utah says the numbers just don’t make sense.
“I think like projects cataloging viruses, doing virus discovery [in wild animals] is interesting from a scientific standpoint,” Goldstein told NPR. “But from the standpoint of predicting pandemics, I think it’s a ridiculous concept.” Because the numbers don’t make sense, Goldstein and others are theorizing that pathogen spillovers may actually happen far more often than we think.
Scientists are unsure how often spillovers occur because they haven’t had the tools or the funding to detect new viruses inside people before they result in widespread illness or pandemics. The existing tests can only detect specific and already known pathogens. In fact, virologist John Lednicky at the University of Florida says that the current panel of tests can only identify the source of an infection about 40% of the time.
“I like to think about it as 60% of the time doctors have absolutely no idea what is causing the respiratory illness,” Lednicky said. This is true no matter where in the world the viral infection occurs. The same panel of tests is used, with the same inability to identify the pathogen in over half of illnesses.
Dr. Gregory Gray, an infectious disease epidemiologist at the University of Texas Medical Branch at Galveston, estimates that unknown viruses are far more common than previously realized. “We probably have novel viruses in North America infecting people who work a lot with animals, especially domestic animals,” Gray says. “We’re just missing them because we don’t often have the tools to pick them up.”
Doctors cannot pick up novel—or new—viruses that haven’t been discovered yet. Several years ago, Dr. Teck-Hock Toh, head of the Clinical Research Centre at Sibu Hospital in Malaysia, began collecting samples from patients who presented with respiratory symptoms. Between 2016 and 2017, Toh collected about 600 swab samples from patients’ noses.
The hospital’s laboratory extracted the genetic material from the pathogens present on the swabs, then froze the samples in liquid nitrogen. Toh was “…looking for novel infections, even types of viruses that we might not be aware of.” What his team found led to a shift in the way scientists and physicians think about searching for the viruses that cause pandemics.
Toh and Gray teamed up to focus their attention on coronaviruses. In 2019, when SARS-CoV-2 emerged in China, scientists only knew of six coronaviruses that could infect humans. These are SARS-CoV-1, transferred from civet cats into people; MERS, which spills over from camels into people; and four other coronaviruses with uncertain animal origins that also cause cold-like symptoms in humans.
Gray estimates that there may be about 1,200 unique coronaviruses that infect a wide variety of animals, including bats, monkeys, rodents, and waterfowl. Using a diagnostic tool that captured all coronaviruses in a sample, the team tested 300 of Toh’s frozen samples for signs of new coronavirus infections. They discovered that about 3% of the patients were infected with animal coronaviruses that had not previously been known to infect humans or lead to pandemics.
Gray called the findings “remarkable” and “hard to believe” especially after the tests hinted that one coronavirus might have come from dogs. At the time, dog and cat coronaviruses were not thought to infect people. Soon, another member of the team performed tests that proved it was a dog virus they had never seen before.
Additionally, the virus’ genes suggested that it could have come from pigs or cats as well, as there was evidence that the virus had exchanged parts of its genome with feline and pig coronaviruses. Further testing in other parts of the world verified the existence of additional animal coronaviruses that had acquired extra mutations to replicate successfully inside human cells.
The conclusion from all of these studies is that spillovers aren’t anywhere near as rare as once thought. This doesn’t mean that rampant pandemics are on the horizon, because the majority of these pathogens cause mild symptoms and hardly ever spread between humans. But learning about the frequency of spillovers may actually help scientists stop future pandemics.